Important: This article is for informational purposes only. Please read our full disclaimer for more details.
Arthritis isn’t only about aging or wear and tear—your daily diet can play a powerful role in either easing or worsening joint pain and inflammation. While no single food can “cause” arthritis, certain foods can intensify inflammation, trigger flare-ups, and contribute to weight gain, all of which place extra stress on your joints.
This expert guide highlights the key foods to avoid and smart swaps that support joint health naturally.
The “Skip List”: 8 Foods That Can Make Arthritis Worse
These foods are known to intensify inflammation, contribute to joint stiffness, trigger flare-ups, or increase body weight—all of which worsen arthritis symptoms. While you don’t need to eliminate all of them, reducing intake can make a noticeable difference in daily joint comfort.
1. Sugary Drinks & Added Sugar
Why it’s Harmful:
Sugary foods such as sodas, packaged juices, sweets, pastries, and desserts cause rapid spikes in blood sugar, promoting an inflammatory response in the body. Excess sugar increases cytokines (inflammation-promoting compounds) and oxidative stress, both linked to worsening arthritis pain.
How Much is Too Much?
- More than 24–36 grams of added sugar per day (approx. 2–3 tablespoons) is considered high and may aggravate symptoms.
Swap with joint-friendly options:
- Water infused with lemon, mint, or cucumber
- Herbal teas or homemade fruit smoothies (without added sugar)
- Dark chocolate (70%+ cocoa) instead of candies
Science insight: A study in the American Journal of Clinical Nutrition found that high sugar intake triggers inflammation and can worsen pain sensitivity (1).
2. Refined Carbs (White Bread, Pasta, Pastries)
Why it’s Harmful:
Refined grains lose their fiber and nutrients during processing. They metabolize quickly, acting like sugar in the body and raising inflammatory markers. They also worsen insulin resistance—a factor linked with systemic inflammation.
Common sources to watch:
- White bread, white pasta, naan, pastries, white rice, crackers, and most breakfast cereals.
Better Alternatives:
- Whole wheat or multigrain bread
- Oats, quinoa, brown rice, barley, or millets
- Whole-grain pasta
Science insight: Research shows that a diet high in refined grains leads to increased CRP (C-reactive protein), a key marker of inflammation that worsens arthritis (2).
3. Processed & Red Meats
Why it’s harmful:
- Red meat (beef, lamb, pork) and processed meats (sausages, salami, bacon, ham, deli meats) are high in saturated fat and AGEs (Advanced Glycation End Products), compounds formed during high-heat cooking. AGEs are strongly linked to chronic inflammation and joint tissue damage.
What to limit:
- Try keeping red/processed meat intake to once per week or less.
Smarter swaps:
- Lean poultry or fish
- Beans, legumes, tofu, paneer
- Grilled or baked options instead of fried
Science insight: Studies in Nutrients and Arthritis Care & Research found that higher red and processed meat intake correlates with increased inflammation and worse arthritis symptoms (3).
4. Fried & Fast Foods
Why it’s harmful:
- Fried foods contain trans fats and refined vegetable oils that fuel inflammation. Fast food meals are also high in salt, calories, and harmful additives, contributing to weight gain—a key aggravating factor for arthritis.
Examples:
- French fries, fried chicken, tempura, pakoras, samosas, burgers, pizza, and convenience fried snacks.
Healthier options:
- Air-fried or baked versions of favorite foods
- Olive or avocado oil for home cooking
- Grilled or steamed meals when eating out
Science insight: High intake of fried food increases CRP levels and inflammatory markers according to multiple studies on diet-induced inflammation (4).
5. Excess Salt & Salty Snacks
Why it’s harmful:
- Too much sodium can cause the body to retain water, contributing to swelling and bloating around joints. Emerging research shows that high salt intake may trigger immune system changes linked to inflammation, particularly in rheumatoid arthritis.
Foods to monitor:
- Chips, salted nuts, pickles, canned soups, instant noodles, packaged snacks, and processed sauces.
What’s a safe intake?
- Ideally, less than 1,500–2,000 mg of sodium per day.
Better choices:
- Unsalted nuts and seeds
- Homemade soups and seasoning blends
- Use herbs, lemon, garlic, and spices for flavor instead of salt
Science insight: Some studies suggest excess salt consumption can worsen autoimmune inflammatory diseases by affecting immune cell activity (5).
6. Certain Vegetable Oils (High in Omega-6)
Why it’s harmful:
- Corn, soybean, sunflower, cottonseed, and generic “vegetable oil” contain high amounts of omega-6 fatty acids. While omega-6 is essential in small amounts, too much—especially without balancing with omega-3—promotes inflammation.
Common sources:
- Restaurant fried foods, packaged cookies, crackers, chips, mayonnaise, and commercially baked goods.
Better alternatives:
- Olive oil or avocado oil for cooking
- Walnut or flaxseed oil for salads
- Increase omega-3 intake to balance (fish, chia, flaxseed, walnuts)
Science insight: A high omega-6 to omega-3 ratio is associated with inflammation and worsening joint pain in arthritis.
7. Alcohol (Especially Excessive Consumption)
Why it’s harmful:
- Alcohol promotes inflammation, increases CRP, and may interfere with arthritis or pain medications. For inflammatory arthritis, heavy drinking may worsen disease progression and joint damage.
Guidance for moderation:
- Limit to no more than 1 drink per day for women and 2 for men, but less is better for arthritis.
If consuming alcohol:
- Choose red wine occasionally (contains antioxidants)
- Avoid binge drinking
- Pair with water to stay hydrated
Science insight: Regular alcohol intake has been linked to chronic inflammation, poor joint recovery, and worsened symptoms in autoimmune arthritis (6).
8. Dairy (For Some People)
Why it’s harmful for some:
- Not everyone with arthritis is sensitive to dairy, but certain individuals report increased joint pain from full-fat milk, cheese, butter, and cream due to saturated fats. Some people with inflammatory arthritis may have a dairy intolerance that contributes to inflammation.
Who may benefit from limiting dairy?
- Individuals with rheumatoid arthritis
- Those who experience digestive issues or inflammation after eating dairy
Better alternatives:
- Low-fat or fermented dairy, like yogurt or kefir
- Plant-based milks (almond, soy, oat)
- Ghee instead of butter (if tolerated)
Science insight: Some studies show dairy can increase inflammation in sensitive individuals, while fermented dairy may have an opposite effect by supporting gut health (7).
Can What You Eat Really Impact Arthritis Symptoms?
Yes—your diet can influence inflammation levels, body weight, gut health, and immune function, all of which affect arthritis. While food alone can’t cure arthritis, nutritional choices can significantly reduce symptom severity. Weight management also plays a role: every extra kilogram increases pressure on weight-bearing joints, worsening pain.
Joint-Friendly Choices: What to Eat Instead
Replacing inflammatory foods with nourishing, anti-inflammatory alternatives can help protect your joints and support mobility.
- Choose whole grains like oats, brown rice, and quinoa over refined carbs.
- Swap red and processed meats for plant-based proteins, eggs, fish, or lean poultry.
- Replace sugary snacks with fruits such as berries, apples, kiwis, and oranges.
- Cook with healthier oils like olive or avocado oil.
- Include fermented foods such as yogurt, kefir, sauerkraut, and kimchi to support gut health.
The Anti-Inflammatory Plate: What It Looks Like
This style of eating focuses on nutrient-dense foods that help reduce inflammation and improve joint health:
- Fatty fish (salmon, sardines, mackerel) for omega-3s
- Colourful vegetables like spinach, broccoli, carrots, and bell peppers
- Berries, grapes, and cherries are rich in antioxidants
- Nuts and seeds for healthy fats (walnuts, flaxseeds, chia)
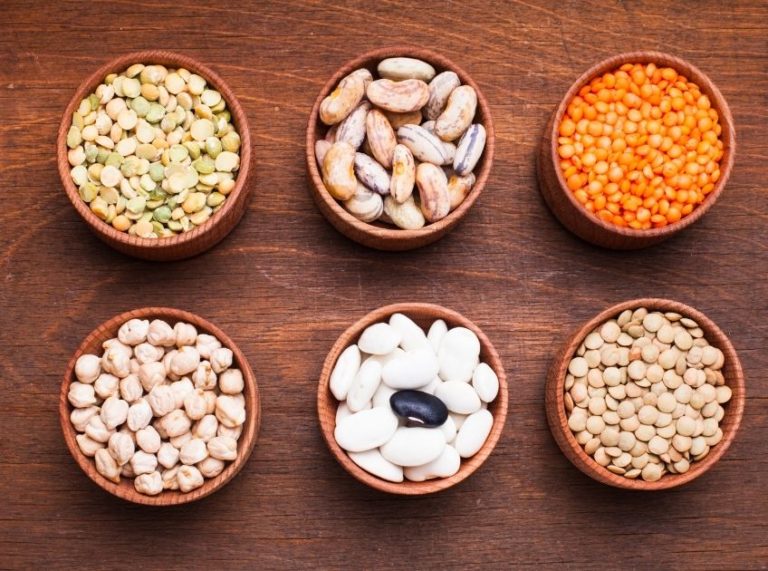
- Legumes such as lentils, chickpeas, and beans
- Herbs and spices like turmeric, ginger, garlic, and cinnamon
Research on anti-inflammatory diets, particularly the Mediterranean diet, shows reduced pain and improved joint function in arthritis patients, with some reporting fewer flare-ups and better quality of life.
Science Spotlight: Why Diet Affects Arthritis
Certain foods trigger inflammation by activating the immune system, increasing oxidative stress, or altering gut bacteria. Anti-inflammatory foods, on the other hand, work by:
- Reducing inflammatory compounds (like CRP and cytokines)
- Providing antioxidants that protect joint tissues
- Supporting cartilage health and reducing oxidative damage
Studies published in The Journal of Nutrition and Rheumatology International show that diets rich in omega-3s, antioxidants, and polyphenols are associated with improved arthritis symptoms and slower progression of inflammatory disease (8).
Frequently Asked Questions (FAQ’S)
1. Are nightshade vegetables bad for arthritis?
A. Tomatoes, eggplants, potatoes, and peppers belong to the nightshade family. There’s no strong scientific evidence that they worsen arthritis for most people, although a small number of individuals may be sensitive. If you suspect a reaction, try an elimination trial for 2–4 weeks.
2. Can supplements help with arthritis pain?
A. Some supplements, such as omega-3 fish oil, turmeric (curcumin), vitamin D, and glucosamine-chondroitin, may offer relief. However, results vary, and supplements should not replace medications. Always consult a healthcare professional before adding new supplements.
3. Does gluten worsen arthritis?
A. For people with celiac disease or gluten sensitivity, gluten can increase inflammation and worsen joint pain. For others, there is no strong evidence that gluten directly affects arthritis. If you notice symptoms after eating gluten-rich foods, a guided elimination trial may be helpful.
You can’t always control arthritis, but you can influence how your body responds to it. Avoiding inflammation-triggering foods while embracing an anti-inflammatory eating pattern can help reduce pain, protect joints, and improve mobility over time.
Small, consistent dietary changes—paired with regular activity, adequate sleep, and medical guidance—can make a big difference in your comfort and long-term joint health.