Important: This article is for informational purposes only. Please read our full disclaimer for more details.
Gout isn’t just a random flare-up of joint pain—it’s a painful inflammatory arthritis caused by a buildup of uric acid crystals in the joints, most commonly the big toe. While genetics, dehydration, and certain medications can contribute, your daily diet plays one of the most influential roles in either triggering a gout attack or helping prevent one.
Foods high in purines (compounds that break down into uric acid) tend to worsen gout symptoms, while others can reduce inflammation and support uric acid removal from the body. Knowing the difference can be a game-changer for anyone trying to control flare-ups naturally.
This guide breaks down the best and worst foods for gout, supported by scientific insights, plus practical eating tips to help you make smarter plate choices.
Gout-Friendly Eating: The Best Foods to Add to Your Plate
These foods may help lower inflammation, reduce uric acid levels, and support joint health.
1. Cherries & Berries
Cherries—especially tart cherries—have been widely studied for their ability to lower uric acid and reduce gout flare-ups. A study published in Arthritis & Rheumatism found that consuming cherries for just two days reduced gout attacks by 35% (1). Their anthocyanins and antioxidants fight inflammation and protect joint tissues. Blueberries and strawberries offer similar benefits.
2. Low-Fat Dairy Products
Skim milk, yogurt, and low-fat cheese have been shown to help reduce uric acid levels. Research in the New England Journal of Medicine demonstrated that low-fat dairy increases uric acid excretion (2). They also provide protein without the purine load of animal meats, making them a smart substitute for high-purine protein sources.
3. Vitamin C–Rich Foods
Citrus fruits, kiwi, bell peppers, and broccoli are excellent for those with gout because vitamin C helps lower uric acid levels. A long-term study published in JAMA found that men who consumed 1,500 mg of vitamin C daily had a 45% lower gout risk than those who consumed less than 250 mg (3).
4. Whole Grains
Oats, quinoa, brown rice, and barley provide long-lasting energy and fiber to support a healthy metabolism. Unlike refined grains, whole grains help stabilize blood sugar—useful since insulin resistance raises uric acid.
5. Leafy Greens & Vegetables
Spinach, kale, cabbage, carrots, zucchini, and cucumbers are packed with antioxidants and low in purines. Contrary to past beliefs, vegetable-based purines do NOT trigger gout attacks. They actually offer anti-inflammatory effects and support healthy weight management, reducing stress on joints.
Foods That Worsen Gout: What to Limit or Avoid
The following foods are high in purines, trigger inflammation, or spike uric acid levels, making gout flare-ups more likely.
1. Red and Organ Meats
Beef, lamb, pork, liver, kidney, and other organ meats are strongly linked to gout flare-ups because of their high purine content. According to BMJ research, red meat consumption significantly increased uric acid levels and was associated with a higher risk of gout (4).
2. Seafood High in Purines
Certain fish—particularly anchovies, sardines, mackerel, herring, and shellfish like prawns—are common triggers. A Harvard study noted that seafood intake increases the risk of gout due to purine breakdown into uric acid (5). If you enjoy fish, opt for salmon or trout occasionally, as they are less problematic.
3. Sugary Drinks & High-Fructose Foods
Soft drinks, packaged juices, energy drinks, and desserts made with high-fructose corn syrup contribute to uric acid overproduction. Unlike glucose, fructose raises uric acid levels rapidly. Research in the British Medical Journal linked sugary drinks to a significant increase in gout risk, especially in men (6).
4. Alcohol (Especially Beer & Spirits)
Beer is one of the biggest dietary triggers for gout due to its yeast and purine content. Spirits also raise uric acid levels. Alcohol interferes with the kidneys’ ability to remove uric acid, causing it to accumulate in the bloodstream. If you choose to drink, wine in moderation is considered less triggering.
5. Processed Foods & Fast Foods
Fried food, packaged snacks, deli meats, sausages, and processed meals are packed with inflammatory fats, refined carbohydrates, salt, and chemical additives. These worsen inflammation and metabolic health—key risk factors for gout. Diets high in processed foods are also associated with weight gain, one of the strongest gout triggers.
The Science Behind Diet & Gout: Why These Foods Affect You
When purines break down, they produce uric acid. Most people can flush this out through their kidneys, but gout sufferers either produce too much uric acid or eliminate too little.
Why some foods worsen gout:
- Animal-based purines produce uric acid rapidly.
- Fructose stimulates uric acid production during metabolism.
- Alcohol reduces uric acid excretion.
- Why some foods help:
- Antioxidants neutralise inflammation and protect joints.
- Dairy proteins promote uric acid removal via urine.
- Vitamin C improves uric acid excretion.
The key is focusing on an anti-inflammatory, low-purine, balanced diet, similar to a modified Mediterranean eating pattern.
Remember:
- Stay hydrated with at least 8–10 glasses of water daily.
- Maintain a healthy weight to reduce pressure on joints.
- Pair dietary changes with regular exercise and medical supervision.
By making mindful food choices and adopting a long-term anti-inflammatory eating pattern, you can significantly improve your quality of life—and keep painful gout attacks at bay.
Frequently Asked Questions (FAQ’S)
1. Can I eat protein if I have gout?
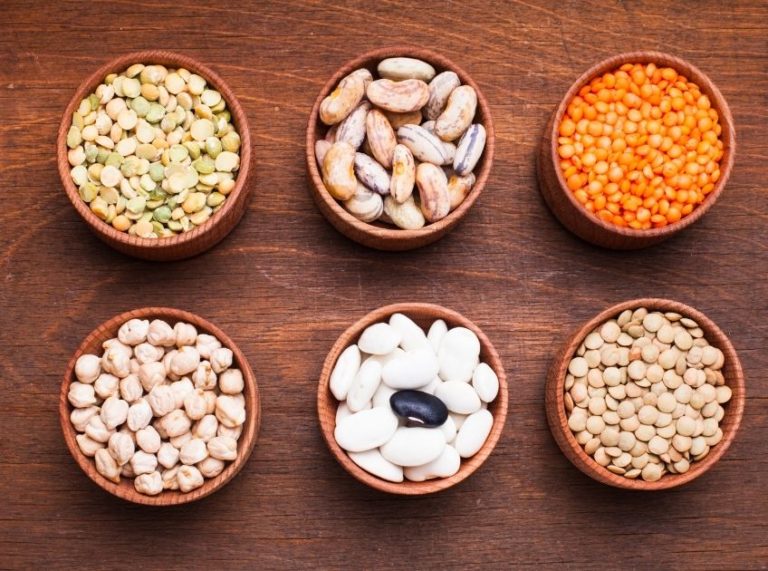
A. Yes. The aim isn’t to remove protein but to choose low-purine protein sources such as eggs, tofu, low-fat dairy, nuts, lentils, and legumes. Fish can be consumed occasionally, but limit high-purine options. Avoid relying on red meat and organ meats for protein.
2. Is coffee good or bad for gout?
A. Moderate coffee consumption may actually help. Studies suggest coffee can lower uric acid levels due to chlorogenic acid and improve insulin sensitivity. However, avoid adding excessive sugar or high-fat dairy creamers. People with acid reflux or anxiety should consider their tolerance.
3. Can gout be managed without medication?
A. For mild cases, dietary changes, hydration, weight management, and lifestyle adjustments may reduce flare-ups. But many individuals need medication such as allopurinol, especially if flare-ups are frequent or uric acid levels remain high. Always seek medical guidance before stopping medication based on diet alone.
Gout isn’t just about what you remove from your plate—it’s equally about what you add. A diet rich in cherries, vegetables, whole grains, low-fat dairy, and vitamin C–rich foods can reduce flare-ups, while limiting red meat, sugary drinks, alcohol, seafood, and processed foods helps keep uric acid under control.